―文献名―
平林優子ら.保育園児の家族が子供の健康に関して利用する社会資源と要望-首都圏1地区の調査より-.2009
―この文献を選んだ背景―
ここ最近、ケアcaféや地域包括ケアシステムなど、地域・コミュニティケアについて重要視され活動も活発になってきているが、対象が高齢者であることが多い。小児に対してはどうなのか、どのようなことが必要とされているのかなど、今後の活動に参考にしたかったため調べてみた。
―要約―
目的
・首都圏の1地区の公立保育園に通院する家族を対象に、子供の健康に関する社会資源の利用状況や要望を明らかにし、地域の支援のあり方を検討する
方法
・対象:首都圏の1地区の公立保育園に通院する1,217家族のうち回答された652件(回収率53.6%)のうち、有効回答649件を分析対象
・調査:調査用紙は2部構成。第1部は全員に回答を依頼し、子供の健康状態、地区の社会資源の利用の実態と要望などを内容とした。第2部は、特に継続支援を必要とする慢性疾患を持つ保護者に回答を依頼し、子供の健康状態、保育園での健康管理と支援の状況、社会資源の利用と利用の困難や要望を内容とした。
・分析:数値や名義尺度に関しては記述統計、記述項目については質問の目的に沿って回答を分類する内容分析を行った。子供の健康問題、社会資源の利用についてはχ2乗検定により慢性疾患の有無で回答の違いを確認した。
結果
・調査対象:回答は母親がほとんど。第2部まで回答した割合は94件(14.4%)。子供の月齢は42.1ヶ月で、2-5歳が77%。男女はほぼ半数ずつ。3-4名の核家族がほとんどを占めた。
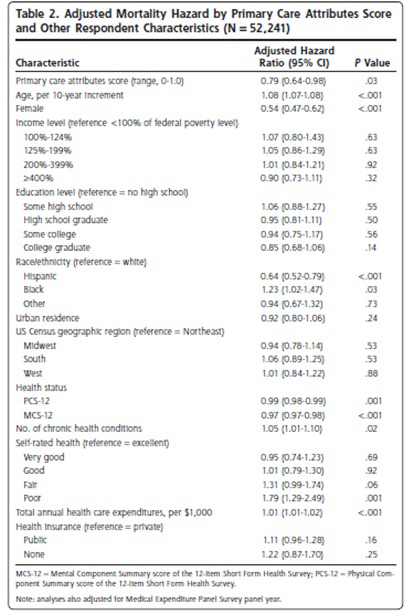
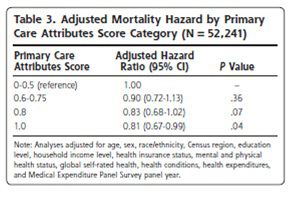
・子供の健康問題(表2):全体では「風邪をひきやすい(32.6%)」が最も多く、次に「アレルギー(27.4%)」が多く、慢性疾患を持つ子供については「気管支ぜんそく(42.6%)」、「食物アレルギー(41.5%)」、「アトピー性皮膚炎(36.2%)」とアレルギー疾患が多かった。
・慢性疾患を持つ子供に必要なケアと保育園での支援の現状(表3):必要なケアについては「毎日の服薬(52.1%)」が最も必要とされていたが、保育園において保育士の支援は行われておらず、毎日服薬が必要な子供の86%が1日2回の服用方法になっていた。外用薬は30%が必要とされていたが、保育士の支援が行われていた。また、支援の現状に関しては「子供の体の状態を観察する(80.0%)」と保育士・看護師からの支援があるとの回答が高かったが、「体の状態に合わせ活動し必要時休息をとらせていない(33.0%)」、「子供のコミュニケーションを助けていない(56%)」という結果であった。
・子供の健康に関連して利用している社会資源と要望
①利用している社会資源(表4):対象の特性から「保育園(80.9%)」は高く、「親族(56.9%)」、「近隣者・友人(52.5%)」、「近所の開業医(53.8%)」、「病院(43.3%)」であり、「インターネット(26.9%)」、「保健センター(19.4%)」と少なかった。また、慢性疾患を持つ子供については「近隣者・友人」の項目のみ有意な差を認め、慢性疾患を持つ子供は「近隣者・友人」を利用する割合が少なかった。また、慢性疾患のみの質問紙の回答では半数近くが「保健師」「保育園看護師」を利用していたが医療者の回答はなく、「医師」についても25%、「病棟や外来看護師」はほとんど回答がなかった。「栄養士(19%)」は比較的高かったが、アレルギー疾患の子供が多いことが関与していると考えられた。
②利用するのに困難がある、あるいはもっと支援を期待したい社会資源:全体的に回答が少なかったが、「保健センター(13.7%)」、「病院(7.7%)」、「近所の開業医(5.4%)」であった。
③子供の健康を守るうえで支援の改善への要望(表5):全334件のうち、種々の社会資源への要望としては「病院・診療所(121件)」が最も多く、診療時間の拡大・小児に対応可能な診療施設の増加が多かった。診療体制に関しては診療内容や対応の改善、待ち時間改善を望んでいた。次に多かったのは「病児・病後児保育や病児がいる際のサポート(80件)」であり、病児保育などを望む声が多かった。「保育園(28件)」については、健康管理機能の充実・健康教育の場・服薬管理という声があり、「保健センター」では対応時間の柔軟性が求められていた。また、「相談システム」については子供の急な病気への相談・気軽に相談できる窓口が求められていた。「予防接種」に関しては予防接種の情報や健診の充実・時間や日程の拡大などが挙げられた。慢性疾患の子供の家族では特に「病児保育の充実」「病院の対応の改善や小児診療の向上」「療養方法の情報提供」などが挙げられた。
―考察とディスカッション―
今回、小児に対する地域・コミュニティケアのきっかけとして上記を調べてみたが、キーとしては「アレルギー疾患」、「慢性疾患の子供を持つ家族」ではないかと感じた。慢性疾患の子供を持つ家族は慢性疾患のない子供を持つ家族に比べ「隣人・友人」を利用する機会が少なくなっているが、「近所の開業医」を利用する人は同等であるということもあり、医療機関としてアプローチできる印象がある。また、その家族を対象としたアプローチや保育園だけではなく、栄養士との連携などもさらにアプローチが広がるのではないかと感じた。皆さんの地域では小児に対する地域・コミュニティケアはどのようにしているでしょうか?
【開催日】
2014年5月14日(水)